|

CYBERONICS
Click on the link to the left to find out more about VNS implants

Do you have an hour to spare? Then, click on the picture
to the left, sit back and watch a video of the complete VNS implant process. (Bear in mind that this is a
pre-recorded video. Therefore, questions cannot be directly submitted to the mediator.)

Is VNS therapy right for you?
Fill out this questionnaire and get some more facts...
VNS
offers hope for epileptics
The VNS has been tested by neurologists and may offer an alternative
for controlling seizures in epileptics for whom drugs or surgery have proven inadequate.
The vagus nerve stimulator, as the device is
called, has yielded promising results in early clinical tests determining its ability to control seizures.
"So far 40 percent of the patients receiving vagus
nerve stimulation have had a 50 percent reduction in seizures, or better," reports Christopher DeGiorgio, associate
professor of neurology and neurosurgery, who heads the Epilepsy Program here.
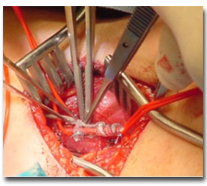
The stimulator, or pacemaker, consists of a
tiny pair of electrodes which are implanted onto the vagus nerve in the region of the neck, and connected to a programmable
generator which is implanted under the skin in the left upper chest.
The surgery to install the device takes a few hours and patients are usually
able to return home in a day.
Other than thin scars on the neck and chest, and a periodic hoarsening
of the voice when the stimulator turns on, patients bear no external signs of having received the implant.
Designed to stimulate the nerve at set intervals of time, the pacemaker
can also be turned on externally by holding a simple magnet over the chest.
The electrodes work by stimulating the vagus nerve, a sensory and motor
originating in the brain stem that enervates a number of organs including the heart, lungs, larynx, vocal cords, stomach,
tongue and ears.
This stimulation in turn, appears to regulate the onset of seizures. "The
cellular mechanisms underlying the effect is still under investigation," said DeGiorgio.
"An epileptic seizure is caused by an abnormal electrical discharge in
the brain," he explained. "We think that stimulating the vagus nerve may abort seizures by activating inhibitory pathways
in the brain. PET studies here at USC show that vagus nerve stimulation activates the thalamus and cerebellum. Inhibitory
pathways may project from these areas to the surface of the brain [cortex] which is where seizures originate.
"To us the vagus nerve is like a freeway which gives us a direct route
into the brain without having to open it up," he remarked.
The original idea for this approach came from experiments conducted by
UCLA neuroscientist Michael Chase about 30 years ago who found that stimulating the vagus nerve in animal models changed the
brain waves. The smaller faster pattern obtained correlated with an anti-convulsive effect, DeGiorgio added.
|
|
| The FDA's stamp of approval on the VNS |

|
| Possible Adverse Effects From the VNS |
____________________________________________________________________
Click on hummingbird to enter a VNS message board

MRIs are off-limits for a handful of implants — mostly pacemakers,
heart-shocking defibrillators, and some brain devices (i.e. VNS).

Click on the Cyber Guy to the right for a copy of the VNS maual
The RNS, unlike the VNS is implanted in the skull &
the electrodes within the brain. It picks up on seizure activity and then goes off by itself.
This explains how it works:
The RNS (about the size of a wallet photo; ≈1.5" X 2.5") is the control center of the process (i.e. the monitoring,
assessing, & treating of it). It's implanted in the patient’s skull just below the scalp and, having a contour
that matches the curvature of the skull, is undetectable once the hair has regrown. In the most common configuration, the
device is connected to two thin electrodes that have been positioned in the area of the brain identified as the focal point,
the point of origination, of the seizure activity. Each of the implanted electrodes contains four contact points used to deliver
small electrical charges.
Once the hardware is in place, the focus turns
to fine-tuning the software. Neurologists begin by establishing a baseline of normal brainwave patterns based on data collected
by the RNS. When the brainwaves spike beyond the normal range, the RNS shows its stuff – within less than a second it
analyzes the feedback, predicts a seizure is about to occur and sends a series of tiny electrical charges that disrupt the
seizure and calm the brain – without the patient feeling even the slightest tingle. A wireless device lets patients
record data captured by the Responsive Neurostimulator to a laptop and then email the results to their neurologist. This data
is analyzed and becomes the basis for future refinements to the RNS settings specially set for each individual patient.
Click to the left to let the people at Neuropace tell you more about how the RNS
functions, resources, clinical trials and contact information
Click to the right to find out about the FDA hearing on February 22, 2013 regarding the
FDA approval of the RNS

Click on the monitor to the left for more information regarding
the RDA webcast discussing the approval of the RNS
|

